Beta Blockers: Effective Antihypertensive Drugs
Beta blockers are also known as β-adrenergic receptor antagonists or blockers. They are effective antihypertensive drugs used to treat hypertension, anxiety, cardiac arrhythmia (irregular heartbeat) and other associated cardiovascular conditions. This document gives a brief information on mechanism of action, therapeutic use, precautions or contraindications and side effects of beta-blockers. Understanding of these aspects will be helpful bot only for healthcare professionals but also for patients to ensure safe and effective utilization of these medications. European Society of Hypertension (ESH) guidelines; Recent (2023) guideline from the European Society of Hypertension (ESH) add β-blockers in the group of effective antihypertensive agents that can be used as first line protocol suitable for initiation of antihypertensive pharmacotherapy. Moreover, can be used in combination with other antihypertensive agents. It is in contrast to the 2018 edition of ESH guidelines. The ESH guideline also recommends the use of β-blockers for patients having resting heart rate (>80 bpm); high resting heart rate is a sign of sympathetic overactivity may lead to the of adverse cardiac remodeling in the setting of hypertension and heart failure. It can be given alone as monotherapy or in combination also. When β-blocker is prescribed, with dihydropyridine calcium channel blocker as combination regimen, these agents reduce both peripheral and central BP. Various studies have shown that the burden of premature morbidity and mortality associated with uncontrolled hypertension, especially strokes can be reduced by combination therapy. What is the Mechanism? Beta-blockers are the competitive antagonist of beta-adrenergic receptors (sympathetic nervous system). they block the action of epinephrine and norepinephrine at beta-adrenergic receptors. These beta-adrenergic receptors are located mainly in the smooth muscles of heart, kidneys, arteries and airways. β1 Receptor Blockade: Blockage of β1 receptors in the heart decrease heart rate, contractility, and cardiac output. It reduces the workload on the heart and normalize blood pressure. these drugs also inhibit the secretion of renin by blocking β1 receptors in the kidneys, a hormone that helps to maintain blood pressure regulation. β2 Receptor Blockade: Bronchoconstriction occurs due to the blocking of β2 receptors cited at the lungs. Avoid the use of non-selective beta-blockers in patients with asthma or chronic obstructive pulmonary disease. some β2 receptors are also situated at blood vessels, and their blockade can lead to vasoconstriction. Classification of Beta Blockers Beta blockers are basically classified according to their activity on adrenergic receptors β1, β2, and β3 receptors, that are as follows: β1 Blockers al; the other name of cardio selective beta blockers. they are mainly found in the heart and kidneys. The most common drugs are metoprolol, atenolol, and bisoprolol. β1 and β2 Blockers also known as non-selective beta blockers as they block the activity of both receptors β1 and β2. Examples are propranolol, nadolol, and timolol. Alpha- and Beta-adrenergic receptor blockers: exert action by blocking both alpha and beta-adrenergic receptors. Examples include labetalol and carvedilol. These drugs are newer and more effective in youngers and lowers high blood pressure that is linked to stress or anxiety. β-Blockers with Intrinsic Sympathomimetic Activity: Few β blockers have Intrinsic sympathomimetic activity (ISA), an activity in which a drug can exhibit both agonist and antagonist properties at a given beta receptor depending on concentration. examples are penbutolol, oxprenolol, pindolol etc. Lipid-soluble beta blockers that can cross blood brain barrier e.g. Propranolol, Metoprolol Water-soluble; that has les CNS effects e.g. Atenolol, Nadolol Indications; Hypertension; Beta-blockers are effective antihypertensive drugs especially in younger patients and those with elevated sympathetic activity. in combination therapy beta blockers reduce both peripheral and central blood pressure. Angina pectoris’ beta-blockers lower myocardial oxygen demand and relieve chest pain due to angina. Heart failure: Some beta-blockers reduce the excessive sympathetic stimulation and improve the survival rate from heart failure. (Bisoprolol. carvedilol, atenolol) Arrhythmias: Beta-blockers help to manage heart rhythm by decreasing the heart rate and the excitability of cardiac tissue (esmolol, sotalol) Glaucoma: Some beta-blockers reduce intraocular pressure in glaucoma patients, Timolol is applied topically to treat glaucoma. Migraine prevention: propranolol & timolol are used prophylactically & treatment of migraine headaches. Anxiety symptoms; beta blockers are used for the symptomatic treatment of anxiety like palpitations and sweating. latest beta-blockers like nebivolol and carvedilol are more effective with fewer side effects. Hyperthyroidism beta blockers are used for the symptomatic treatment of hyperthyroidism like rapid heart rate and severity of tremors Akathisia; a movement disorder often associated with the use of antipsychotics (propranolol, metoprolol) Side Effects Central nervous system-associated side effects Fatigue or tiredness, confusion, nightmare, restlessness. hallucination, depression, insomnia, Parkinsons disease, psychosis Orthostatic or postural hypotension GIT nausea, vomiting, diarrhea Alteration of glucose & lipid metabolism (β1-blockers) Respiratory bronchospasm. dyspnea especially in asthma or COPD (more common with non-selective beta-blockers), Electrolyte disturbances; Hyponatremia, hyperkalemia (beta-1 receptor) long term side effects of beta blockers include Cold Extremities, Erectile Dysfunction, insomnia or sleep loss, difficulty to concentrate or focus, frequent mood changes, short term memory loss, a little weight gain of about 2-4 pounds. Precautions and Contraindications; It is absolutely contraindicated in hypotension, Bradycardia, cardiogenic shock, acute bronchitis, bronchospasm, Dose; Doses depend on various factors like medical condition, patient’s demographics and condition of patient. some common doses along with drugs are as Metoprolol tartrate: 25–100 mg orally 12hourly (can also be given IV, 100 mg daily in single or divided doses) Metoprolol succinate tablets/ capsule (extended-release): 25–200 mg once daily for both adults & children orally Atenolol: 25–100 mg once daily for Hypertension, angina, arrhythmias Propranolol: 40–80 mg 2-3 times a day (or extended-release 80–160 mg once daily) Timolol gel & eye drops Labetalol is the beta blocker that can be used in pregnancy induced hypertension. 0.004% of the original dose is secreted in milk, so nursing mothers should consult health care professionals. FAQ What are beta blockers? Beta blockers are the medications that lowers blood pressure, heart rate & other cardiovascular issues by blocking beta adrenergic receptors. they are used to treat many conditions like chest pain due to angina, migraine, anxiety, cardiac arrhythmia etc. Which beta blocker is best prescribed in younger people? It depends on medical
ACE inhibitors (Angiotensin-converting enzyme inhibitors)

ACE inhibitors (angiotensin-converting enzyme inhibitors) are a type of medicine that is mostly used to treat hypertension and heart diseases by relaxing blood vessels. ACE inhibitors blocks the activity of angiotensin-converting enzyme, which do not allow the conversion of angiotensin 1 into angiotensin 11. Moreover it also increases the levels of a peptide bradykinin that lowers blood pressure by opening blood vessels. All of the ACE inhibitors are available in oral dosage form except enalapril, that is available oral & intravenous injectables. FDA has approved ten angiotensin-converting enzyme inhibitors till date . Captopril was the first approved in 1981 by FDA for hypertension. Others are Enalapril, Lisinopril, Ramipril, Trandolapril, foscinopril, perindopril, quinapril, benazepril moexipril. On the basis of the chemical structure, angiotensin-converting enzyme inhibitors can be classified into three groups. yjat are Sulfhydryl-containing ACE inhibitors (Captopril) Phosphorus-containing ACE inhibitor (Fosinopril) Dicarboxylic-containing ACE inhibitors (Enalapril, Lisinopril etc) Mechanism of action Primary mode of action of angiotensin-converting enzyme inhibitors involves the suppression of the angiotensin-converting enzyme (ACE), which is necessary for the renin-angiotensin-aldosterone system. ACE inhibitors (angiotensin-converting enzyme inhibitors) blocks the conversion of angiotensin I angiotensin II. Angiotensin II is a strong vasoconstrictor that elevates blood pressure by making blood vessels smaller. ACE inhibitors controls blood pressure and enables the heart to work less by reducing the levels of angiotensin II. The reduced levels of angiotensin II opens up blood vessels, lowers blood pressure and makes the heart work less. ACE inhibitors (angiotensin-converting enzyme inhibitors) also lowers the secretion of aldosterone from adrenal glands. It makes the body hold onto less sodium and water and lowers blood volume and pressure. ACE inhibitors also inhibits the metabolism or breakdown of a peptide named bradykinin that lowers blood pressure by opening blood vessels. However the higher levels of bradykinin may create side effects like hypotension, dry cough, electrolyte imbalance or angioedema. Many drugs belong to this group. however differ a little in mechanism of action, the side effects they cause. All work much the same to lower blood pressure and protect the heart and kidneys. Indications For the treatment of high blood pressure in adults the Eighth Joint National Commission (JNC8), published evidence-based guidelines in 2014. These guidelines recommended ACE inhibitors as one of the four drug classes that can be used as initial therapy in hypertension. According to the American Heart Association/American College of Cardiology (AHA/ACC) and the European Society of Cardiology (ESC) guidelines 2023, angiotensin-converting enzyme inhibitors can be used as first-line antihypertensive protocol, preferably for the patients suffering with chronic cardiovascular diseases & diabetes mellitus. ACE inhibitors reduces the progression of disease nephropathy in Type 1 (insulin-dependent diabetes mellitus) and greatly lower the risk of death, dialysis, and transplantation. ACE inhibitors stop microalbuminuria from getting worse and turning into overt proteinuria. They also stabilize kidney function in people who have never been treated before and have compromised kidney function. Heart attack or myocardial infarction left ventricular systolic dysfunction Adverse Effects Common Adverse Effects; Dry cough, headache, fatigue, weakness, diarrhea, nausea, dizziness, Hypotension ACE inhibitor-induced dry non productive cough is more common among women than men. Reduced glomerular filtration rate GFR, & higher serum creatinine is observed in approximately 30%. It become more significant when diuretics and NSAID s are administered along with ACE inhibitors (angiotensin-converting enzyme inhibitors). One-fifth of the patients suffering with renal artery stenosis may develop elevated levels of BUN in blood urea nitrogen and creatinine levels. This decline in renal function is reversible & stabilizes within 2-4 weeks. Angioedema, most significant adverse effect that can affect any part of the body however tongue, glottis or larynx mostly effected & cause airway obstruction. Rate is high in African-American population. Many drugs like epinephrine. diphenhydramine, methylprednisolone & bradykinin blocking agents can be used. However in case of airway compromise , the airway along with an endotracheal tube is applied that allows ventilation. Hyperkalemia especialy Cholestatic jaundice or hepatitis or hepatic necrosis in rare cases Although the efficacy of Angiotensin receptor blockers (ARBs) & ACE inhibitors are similar but later has a higher incidence of side effects like cough and angioedema. this is the reason that some clinicians prefer to prescribe ARBs. over angiotensin-converting enzyme inhibitors. Hematologic disorders like neutropenia, agranulocytosis and other blood dyscrasias may occur. Precautions to use ACE inhibitors (angiotensin-converting enzyme inhibitors) Concomitant administration of ACE inhibitors and co-trimoxazole may cause mortality (sudden death) due to hyperkalemia. ACE inhibitors are contraindicated in patients with a history of angioedema or hypersensitivity. Monitor if signs of angioedema appear, like swelling of the face, lips, tongue, or throat, stop its use & seek immediate medical attention. It should not be given to patients already taking a direct renin inhibitor such as aliskiren. It should not be given to patients cardiac outflow obstruction It should not be given to patients with hypovolemia or dehydration ACE inhibitors should not be given during pregnancy due to the risk of fetal harm as it may cause congenital malformations, neonatal death or still birth, . Women planning to conceive or who become pregnant should consult physician prior use. The combination therapy of ACE inhibitors with other antihypertensive drugs especially ARBs & potassium-sparing diuretics can worse renal indices, hypotension and life-threatening hyperkalemia. Avoid if you have a known allergy to ACE inhibitors. High potassium levels or creatinine or decreased glomerular the drug needs to be adjusted accordingly or discontinued. Dosage form & Dose All of the ACE inhibitors are available in oral dosage form except enalapril, that is available oral & intravenous injectables. FDA has approved ten angiotensin-converting enzyme inhibitors till date . Captopril was the first approved in 1981 by FDA for hypertension. all have some differences regarding its uses , mechanism or side effects but they all work the same to decrease blood pressure and protecting the heart and kidneys. Some doses of ACE inhibitors for hypertension are as follow Captopril: Tab 25 mg. start dose 12.5–25 mg bid-tid with a maximum daily dose of 150mg Enalapril: Tab 5 mg. initial dose 5 mg , a maximum daily dose of 40 mg
Amlodipine besylate
Amlodipine besylate is a common calcium channel blocker (CCB) that is mostly used to treat high blood pressure and chronic stable angina (chest discomfort). It is a calcium antagonist and belongs to the dihydropyridine class, which means it relaxes blood vessels and makes blood flow better. It was approved for medical use in 1990 and included in the essential medicine list of WHO. According to a report of 2022, it was the fifth most commonly prescribed medication for hypertension in the United States of America. Amlodipine is a good choice for treating high blood pressure because it has a lengthy half-life of 30 to 50 hours and only needs to be taken once a day. The bioavailability of amlodipine besylate is 64% to 90% & plasma concentrations is achieved in 6 to 12 hours. Amlodipine is metabolized by the liver to inactive metabolites and excreted by kidneys. Mechanism of action of Amlodipine involves a number of important steps Being peripheral arterial vasodilator, it stops calcium from getting into smooth muscle in arteries, causes vasodilation, which lowers systemic vascular resistance and blood pressure. By stopping calcium from getting into cells, amlodipine opens up coronary arteries, which makes it easier for the heart to get oxygen, especially in people with vasospastic angina. It binds to the alpha1 subunit of L-type calcium channels, prevent its opening. It reduces the entry of calcium ions and modifies the contractility of the heart and smooth muscle. All of these mechanisms work together to make amlodipine effective for treating high blood pressure and angina. What Amlodipine besylate is used for High blood pressure (hypertension) Reduces peripheral vascular resistance by relaxing the smooth muscle in the arteries, which lowers blood pressure. By opening up the coronary arteries, it increases blood flow to the heart and lowers the number of angina episodes. Chronic stable angina (due to physical or emotional stress) Vasospastic angina Often used as a first-line treatment, either by itself or with additional antihypertensive medications. Helps to stop spasms in the coronary arteries that cause chest discomfort. A new study suggests that amlodipine, can help to manage ADHD symptoms as it significantly reduced hyperactivity when used on rats and zebrafish. Dose & dosage form of Amlodipine besylate It is available in oral dosage form i.e. Tablets of 2.5mg, 5 mg and 10 mg. In adults: Initially, a dose of 5 mg/day is recommended once a day & should not exceed 10 mg/day. In children and adolescents (6 to 17 years of age), the initial dose of 2.5 mg once a day is the recommended dose. Children under six years initial dose is 0.05-0.1 mg/kg/day & can be raised a maximum dose of 0.6 mg/kg/day after a week. People over 65 or with liver problems may start with 2.5 mg/day. For angina patients, first dose is 5 mg once a day. The maintenance dose will be 5 to 10 mg once a day, with a maximum dose of not more than 10 mg per day. Amlodipine besylate can be taken with or without food, but better to take at same time to get best results. It should be taken with a glass of water. Warnings and Things to Avoid Amlodipine besylate is usually well-tolerated, however there are several things you should do to be safe Hypotension (low blood pressure) can cause blood pressure to drop too much, especially in patients who are low on volume. Severe Aortic Stenosis: Be careful when using it because it can lower blood flow to the heart. Liver damage: You may need to change the dose since your metabolism is slower. Heart Failure: Be careful when giving Calcium channel blockers to those with heart failure, as they may make symptoms worse in some circumstances. Pregnancy (Category C): Only use if the benefits are greater than the hazards. Breastfeeding: A little quantity of the drug comes out in breast milk. Talk to your doctor before using it. Keep all medication out of sight and reach of children as many containers are not child-resistant. and away from light, excess heat and moisture Always lock safety caps. Place the medication in a safe location – one that is up and away and out of their sight and reach. Dispose of unneeded medications side effects of Amlodipine besylate Most side effects are mild to moderate, but some may need medical help Common side effects of amlodipine besylate include peripheral oedema (which is swelling in the ankles and feet) migraines, hypotension etc Some adverse effects are related to dose like dizziness, weakness, palpitations, and hot flushes. Rare effects include jaundice, pancreatitis, hepatitis or cholestasis and high levels of transaminases. Allergic reactions, erythema, pruritus associated with amlodipine that disappear with the discontinuation of treatment. Chest discomfort that gets worse (not often, but can happen in angina patients) Amlodipine-associated gingival overgrowth. symptoms of overdose may include dizziness, tachycardia, fainting & severe low blood pressure. It can be treated with fluid replacement and maintaining glucose levels. Need to monitor patient s vital signs, respiratory system function, blood glucose levels, renal function and urine output. Interactions between drugs Amlodipine besylate can change how other drugs work, when taken together: Amlodipine may raise the levels of simvastatin (don’t take more than 20 mg/day of simvastatin). Strong CYP3A4 inhibitors, such ketoconazole, itraconazole, and clarithromycin, are: Increase the amount of amlodipine in your body, which raises the chance of negative effects. Other antihypertensives, like beta-blockers, ACE inhibitors, and diuretics, may make the blood pressure-lowering effects stronger, which raises the risk of low blood pressure. Grapefruit juice may help the body absorb amlodipine better, which can raise blood levels. If you are taking other medicines either prescribed or over the counter, inform your doctor and pharmacist. Dose of amlodipine may need to change, or careful monitoring may be required.You must inform your healthcare professional if you ever had heart or liver disease. Amlodipine besylate is a good and often given medicine for high blood pressure and angina. It just needs to be taken once a day and is
Hypertension (high blood pressure)
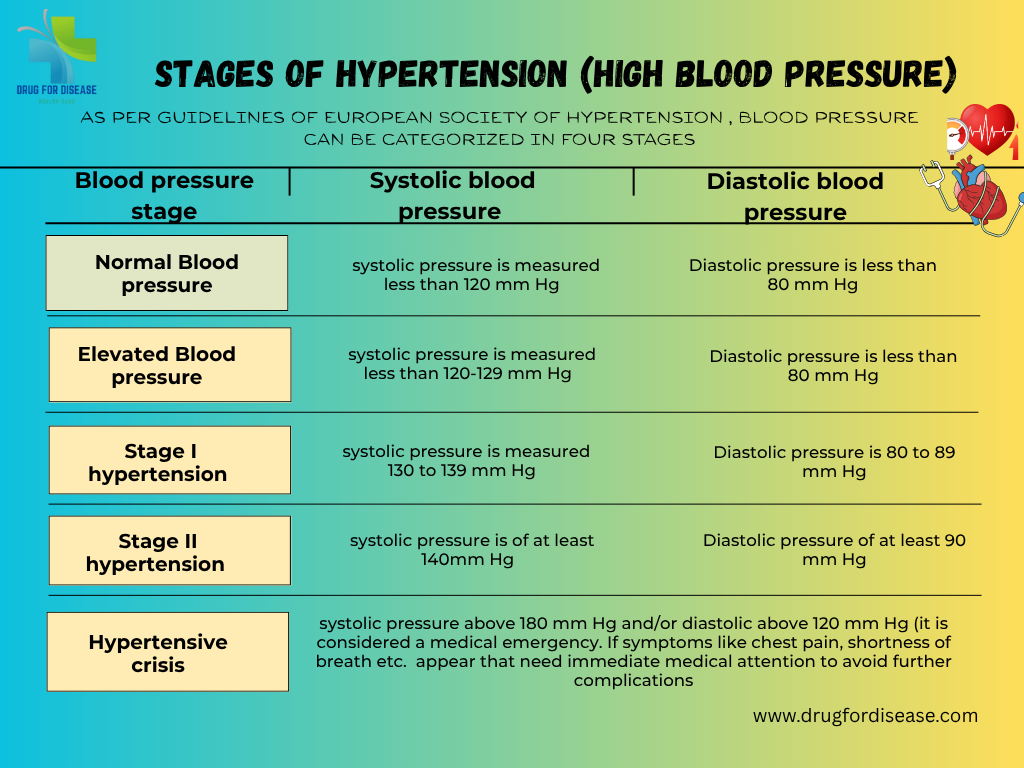
Hypertension or high blood pressure is the most common non communicable disease that appears when the force (pressure) of blood against the artery walls is continuously high. Or in other words consistent raised arterial pressure is termed as hypertension. How to take readings of hypertension Hypertension or high blood pressure is measured by two values that are systolic pressure & diastolic pressure. Systolic blood pressure represents the pressure of blood in arteries when heart beats & diastolic blood pressure is the pressure of blood is on artery walls when the heart muscle rests between beats. A normal blood pressure value is 120/80 mmHg. Hypertension or high blood pressure is usually diagnosed when blood pressure consistently exceeds 130/80 mmHg. Globally1.28 billion adults between the age of 30–79 years are suffering from hypertension. About two-thirds of hypertensive cases belong to low- and middle-income countries. It is the major cause of premature mortality (WHO, 16 March, 2023). Stages of Hypertension or high blood pressure As per European Society of hypertension guidelines, blood pressure can be categorized in four stages Normal Blood Pressure: systolic pressure is less than 120 mm Hg while diastolic is less than 80 mm Hg Elevated Blood pressure: systolic pressure of 120-129 mm Hg and diastolic less than 80 mm Hg, need to consult health care professional to manage the condition. Stage 1 Hypertension: systolic pressure of 130 to 139 mm Hg or diastolic of 80 to 89 mm Hg. It can be managed by lifestyle changes and medication. Stage 2 Hypertension: systolic pressure of at least 140 mm Hg or diastolic of at least 90 mm Hg or above. Hypertensive crisis: systolic pressure above 180 mm Hg and/or diastolic above 120 mm Hg (it is considered a medical emergency. Following symptoms may appear, that need immediate medical attention to avoid further complications chest pain, shortness of breath, difficulty in speaking, numbness, weakness, blurred vision etc. Types of Hypertensions (high blood pressure) Hypertension or high blood pressure is basically classified into two major types, that are Primary /Essential Hypertension; It is the most common type, affecting between 90 to 95 percent of people. It develops slowly over time and has no known cause, but linked to behavioral factors, genetic, environmental factors, diet, smoking, excessive salt intake, less physical activity etc Secondary Hypertension Secondary Hypertension or high blood pressure is affecting 5–10% percent of people worldwide. It occurs suddenly and is due to an underlying medical condition or conditions like adrenal gland tumors, thyroid problems, stroke, kidney failure, birth control tablets or medicines etc. Secondary hypertension is more prevalent in younger people & 30% of people have an age of 18 to 40 years. Other Subtypes of hypertension include Isolated Systolic Hypertension Mostly older people suffer with isolated systolic hypertension. Blood pressure ranges from 140- 90mmHg systolic pressure and diastolic pressure respectively. Malignant Hypertension (Hypertensive Emergency Blood pressure rises quickly and severely (typically >180/120 mmHg. It may cause damage to one or more organs like kidney, lungs, brain etc. symptoms.like confusion, anxiety, drowsiness, chest pain, and shortness of White Coat Hypertension: Elevated blood pressure only in clinical settings due to anxiety while patient gets normal at home Masked Hypertension; It is the vice versa of above readings is normal in clinical settings but elevated at home or in daily life. Gestational hypertension Hypertension occurs in approximately 8–10% of pregnancies after 20 weeks of gestation and women have a blood pressure higher than 140/90 at two readings with at least 6 hours gap Other pregnancy related hypertension or high blood pressure are Pre-eclampsia & Eclampsia that need special care and emergency treatment. Causes & Risk Factors of hypertension or high blood pressure No physical activity unhealthy diet that are rich in salt, sugar, saturated and trans fats, carbonated drinks, etc. smoking tobacco or being exposed to secondhand smoke that may damage blood arteries and cause high blood pressure. excessive salt intake anxiety or stress Being overweight or obese Family history or genetic factors Age and sex Adrenal tumors (e.g., pheochromocytoma) Medications (NSAIDs, steroids, birth control pills Chronic kidney disease Hyperthyroidism or hypothyroidism COMPLICATIONS OF HYPERTENSION Coronary heart disease (CHD) Myocardial infarction (MI) Stroke (CVA), either ischemic or intracerebral hemorrhage Hypertensive encephalopathy Renal failure, acute versus chronic Peripheral arterial disease Atrial fibrillation Pathophysiology & Diagnosis Increased salt absorption resulting in volume expansion Increased activation of the sympathetic nervous system An impaired response of the renin-angiotensin-aldosterone system (RAAS) It can be diagnosed by routine blood pressure monitoring with electronic or manual BP apparatus sphygmomanometer, blood tests (renal function, electrolytes, lipid profile), urine test etc. Treatment Plans Lifestyle Modifications Medications: Preferred drugs are Diuretics, Calcium channel blockersm ACE inhibitors, Beta blockers Identify and treat the underlying cause Adjust or stop contributing medications Hypertension or high blood pressure is often silent but deadly. Early detection, lifestyle changes, and appropriate treatment can prevent serious complications. Everyone over the age of 30 should monitor their blood pressure regularly—even if they feel healthy.

